Radiofrequency ablation is a pain management procedure. When performed, an electrical current is produced by a wave to heat up an area of nerve tissue. Therefore, decreasing pain signals from that area. Allowing you to properly manage pain.
Radiofrequency ablation has helped those with chronic lower back and neck pain. However, it is also used to treat degeneration in joints in arthritic patients.
This procedure, however, allows for about six to twelve months of pain relief. Although it does vary from patient to patient. Additionally, it also depends on the severity of the pain and the location.
How safe is radiofrequency ablation?
This procedure is a safe and effective way to treat pain. As mentioned before, effects vary from patient to patient. But it is typically well-tolerated. However, this is a slight risk of infection at the insertion site. This procedure is not for everyone, though.
As with many other medical procedures, RFA may is not the right choice for everyone. For example, some people who have an active infection or bleeding issues. Therefore, they may not qualify for radiofrequency ablation. As always, speak with your doctor before a procedure about any possible interactions with current conditions or diseases.
The main side effect of radiofrequency ablation is discomfort. And this would include swelling and bruising at the site of the treatment. But, this generally subsides within a few days.
What Happens During Radiofrequency Ablation Procedure?
In the field of pain management, and specifically in pain managing of spine-related pain, RFA has exploded in recent years and with excellent patient outcomes. RFA (rhizotomy) treats severe chronic joint-related pain, in areas such as:
- low back (lumbar spine)
- mid-back (thoracic spine)
- neck (cervical spine)
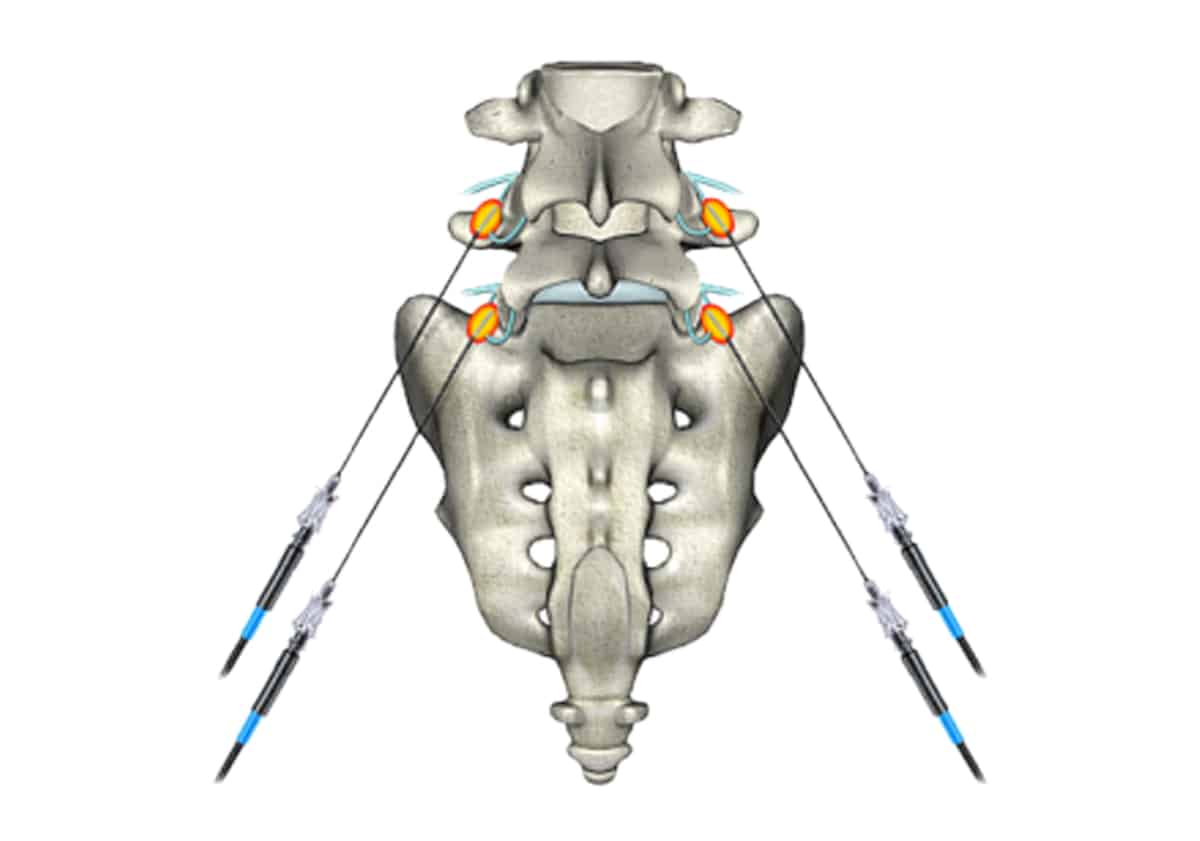
- sacroiliac joints
In these regions of the spine, radiofrequency waves apply heat to the medial branch nerves. And the medial branch nerves are surrounding the spinal facet joints. These facet joints are the articulating joints in the spine. Which, much like other joints in the body, consists of two bones articulating via a fluid-filled joint space and surrounded by a “synovial” joint capsule. These joints are what allow the human skeleton to flex, extend, and rotate. In fact, just the same as other larger joints in the body. But they are equally prone to developing arthritis and causing pain. Many people believe facet joint arthritic pain to be an under-diagnosed pain condition.
How To Treat the Arthritic Spinal Pain
The first step in treating this arthritic spine pain is establishing a specific diagnosis. This is the key to the correct and safe utilization of RF technology. So, in this procedure, a pain specialist performs a facet joint block. Then, the pain specialist uses an x-ray machine called a fluoroscope to identify the specific facet joints. Then, subsequently injects a local anesthetic, or numbing agent, directly into the target area. And the target area is usually the anatomical location of the medial branch nerve.
In fact, people believe the nerve carries the “pain signal” directly from the arthritic facet joints to the spinal nerves, spinal cord, and brain. Now, if a facet joint injection results in a greater than 50% reduction in the patient’s pain, then RF is usually an appropriate next step in the treatment plan. Some practitioners, however, will perform a second diagnostic facet injection before proceeding with the actual RFA.
The radiofrequency ablation procedure is similar to the facet block itself. But, instead of using special RF needles. These RF needles have tips containing specific RF probes and generate heat through the needle-tips.
First, needles are placed using the same x-ray guided technique as the facet block, and the active RF probes are inserted through the needle cannulas. Next, a safety check (before the actual RF or heating procedure.) During which they are stimulated at different frequencies, normally 50Hertz and 2Hertz. Next, the physician and patient establish that reproductive stimulation, that is felt at the specific location of their spine pain.
What Happens Next?
After this safety check, an anesthetic agent is injected. This numbs the structures before the RF or heating process. Now, the RFA is performed at a temperature of 80 degrees centigrade for 60 to 90 seconds. Therefore, generating heat around the nerve, though its ability to transmit pain signals to the brain is destroyed. Thus, ablating the nerve. After the RFA procedure and just before the needles are removed. However, some practitioners inject a steroid to aid with the healing process and prevent a pain “flare-up” that rarely occurs.
Now, the patient can go home. Almost instant pain relief is typical. However, mild discomfort is common.
RFA is a minimally invasive procedure and is performed in the office. The patient is awake during this. Avoiding risks associated with general anesthesia. RFA is an excellent treatment for arthritic related spine pain. Always make sure you are in the hands of an experienced pain practitioner, though. However, pain relief lasts from 6 to 12 months. Since the medial branch nerves do regenerate over time. Therefore, pain tends to eventually resurface.
Is RFA a Long Term Solution?
RFA is a longer-term solution than many other pain procedures and is a less invasive option than spine surgery. Spine pain stemming from facet joint arthritis is a largely under-diagnosed pain condition and can be successfully managed with RFA. Ask your pain doctor if RFA might be appropriate for you.
Our spine specialists and pain management doctors at Spine and Orthopedic Center is here to help. If you are experiencing back pain or neck pain, call us at 888-409-8006. Our offices are conveniently located throughout South Florida.






Leave A Comment